Being stressed is something that you can probably relate to. However, have you ever put any thought to how stressed your bones might be?
Normal day-to-day activity places a certain level of stress on your bones – this is generally healthy and helps keep your bones strong.
Failure to stress your bones much (i.e. lack of physical activity and minimal incidental activity with day-to-day activity) can contribute to loss of bone density and in time osteoporosis.
Physical activity (especially of the weight-bearing kind) places additional stress on your bones. In most circumstances, your body will respond to this activity load and stress to become stronger and more resilient to higher levels of activity (bone stress) in the future.
Repeated bouts of physical activity or weight-bearing activity, especially if for prolonged periods of time or repeated regularly without adequate periods of rest in between, can lead to over-stressing your bones. Initially this will result in a bone stress reaction, which is where there is oedema (or swelling within the bone) and can be painful. If the bone is continued to be stressed, this can result in a stress fracture!
We see lots of people in the clinic with varying degrees of bone stress reactions & stress fractures. Identifying a bone stress reaction or fracture ASAP is incredibly important, as continuing to place stress on the bone can worsen the injury. Most of these injuries require rest from activity for a certain period of time as part of the required treatment. The worse the bone stress reaction or if a stress fracture has occurred the longer the required period of rest and this may require you to be non-weight bearing which can have considerable impact on work, physical activity and day-to-day activities.
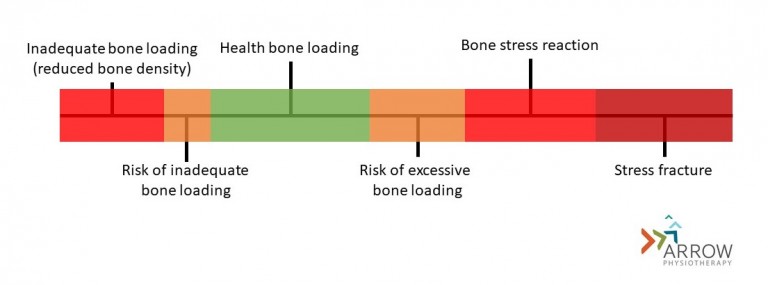
As you can see, bone stress to some extent in normal and actually healthy. It is a continuum and you ideally want to be stressing your bones enough to keep them healthy and strong to be able to tolerate the level of activity that you do whether that be with day-to-day activities or sporting/recreational pursuits.
How would I know if I had a bone stress reaction or stress fracture?
It can often be difficult to differentiate a bone stress reaction or fracture from other injuries – many people will often think that they have a muscle strain or some general post-exercise soreness. There are some key defining features of most stress reactions/fractures:
- Completion of regular weight-bearing activity or exercise in the lead up to onset of symptoms. This is usually at a higher intensity, duration or frequency than previous levels of activity.
- Pain tends to be present during activity that places stress through the bone and gets worse as activity is continued.
- Pain eases after activity, although may linger as the condition worsens (lingering pain especially at rest typically is associated with more significant stress reactions or stress fractures).
- Pain tends to be quite focal initially and if left to worsen often becomes more disperse.
There are a number of other factors which can influence the likelihood of sustaining a bone stress reaction or stress fracture. These include:
- Reduced bone density, hormonal factors & low body mass are all associated with an increased risk of bone stress reactions/fractures.
- Various anatomical differences can increase the risk of certain bone stress reactions/fractures e.g. reduced foot arch height and shin stress injuries.
- Certain sports are associated with particular types of bone stress injuries:
- Running sports/walkers – feet & shins
- Rowing – rib
- Cricket fast bowlers & gymnasts – lumbar spine
- Dancers – feet
- Retail workers (or people standing on their feet for considerable period of time) – feet & shins
- Other factors can include activity technique, footwear, surface on which activity is performed.
What should you do if you think you may have a bone stress reaction/fracture?
It is incredibly important to get an accurate diagnosis, such that you know whether you do have a bone stress injury and how bad it is. It is also important to know exactly which bone is involved, as different bones require different treatment and differing time-frames to heal. Different bones also have different risk factors which also need to be looked at to ensure that once the injury has healed, that you don’t sustain it again in time.
So, it is incredibly important to see a health professional who has lots of experience in assessing and managing bone stress injuries (we can help with this! Click here to make an appointment for us to assess your bones). If it is suspected that you do have a bone stress injury, you will likely be sent for some form of imaging to help confirm the injury. In most cases this will require an MRI or bone scan. Xrays are not good for looking at bone stress injuries – they only show stress fractures when they are really bad (we often find that people are sent for these to rule out bone stress injuries – they don’t!!).
What treatment is needed for a bone stress reaction/stress fracture?
The treatment required is dependent of the extent of bone stress injury, which bone is involved and whether there are any underlying contributing factors to address. In general, all bone stress reactions will require a period of reduced activity (so as not to continue to stress the bone) – the extent of injury will dictate the length of time for this and how extensively activity needs to be reduced. Once the symptoms have settled and there is evidence of healing, activities that stress the injured bone are gradually re-applied. Whilst the above management of the injury is being conducted, it is important to address any contributing factors to ensure (or reduce the likelihood) that the injury doesn’t reappear – this can be checking bone density, working with coaches to better manage activity load, addressing strength/biomechanical/technique issues or fixing footwear.
From everyone at Arrow Physiotherapy, we hope that you are stressing your bones adequately to keep them strong and healthy, but hopefully staying short of over-stressing them!